Scientists have identified how misfiring of the immune response in COVID-19 patients can lead to severe consequences of the disease, a tool that may help identify those at high risk of the disease and suggest drugs to treat them.
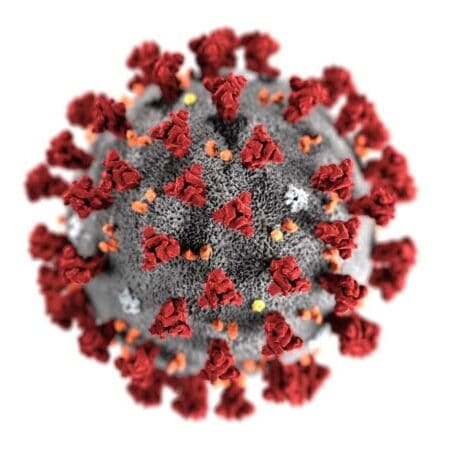
SARS-CoV-2, the novel coronavirus that caused the disease COVID-19 affects different people differently. There exists a broad range of clinical symptoms, as well. Numerous reports have indicated that coronavirus, including Severe Acute Respiratory Syndrome Coronavirus (SARS-CoV), and Middle Eastern Respiratory Syndrome (MERS), elicits an aggressive immune response in many patients (Chen et al., 2007, Jose et al., 2020).
A new study by Yale scientists, published July 27 in the journal Nature, reports that analyzing differing immune system responses of COVID-19 patients can help predict who will experience moderate and severe consequences of the disease (Lucas et al., 2020).
The findings may help identify patients at high risk of severe illness during the period of their hospitalization and suggest drugs to treat the disease.
Researchers examined 113 patients admitted to Yale-New Haven Hospital, and serially analyzed the different immune system responses parameters in patients with moderate (non-ICU) and severe (ICU) disease.
They found that all patients shared a typical pattern in immune system activity early in the disease. However, individuals who experienced only moderate symptoms exhibited reduced immune system responses and viral load over time.
Patients who developed severe symptoms showed no decrease in viral load or immune system reaction, and many of the immune signals in these patients accelerated.
Following an early increase in cytokines, patients with moderate cases displayed a progressive reduction in type-1 (antiviral) and type-3 (antifungal) responses.
In contrast, patients with severe conditions maintained these elevated responses throughout the disease. Moreover, the severity of the situation was accompanied by an increase in multiple type 2 (anti-helminths) effectors, including IL-5, IL-13, IgE, and eosinophils.
Researchers found indicators that predicted which patients were at the highest risk of developing severe forms of the illness in the early course of treatment. One risk factor was the presence of alpha interferon, a cytokine mobilized to combat viral pathogens such as the flu virus.
However, COVID-19 patients with high levels of alpha interferon fared worse than those with low levels. Another early indicator of poor outcomes is the activation of the inflammasome, a complex of proteins that detects pathogens and triggers an inflammatory response to infection. Inflammasome activation was linked to poor results and death in several patients.
Researchers found that people who respond better to the infection tend to express high levels of growth factors, a type of cytokine that repairs tissue damage to the linings of blood vessels and lungs.
In conclusion, the data can help predict patients at high risk of poor outcomes. The drugs that target specific causes of inflammation identified in the study could help treat patients at risk of developing severe cases of COVID-19.



















