COVID-19 survivors exhibit a higher risk of death and use of health resources beyond the first 30 days of illness. The latest evidence indicates that a substantial burden of health loss that extends from lung to other vital organ systems is experienced by patients who survive after the acute phase of COVID-19.
COVID-19, a viral disease, is caused by the coronavirus SARS-CoV-2. Since its emergence in Wuhan, China, in 2019, the virus has infected over 200 million people leaving 4,288,871 deaths as of May 6, 2021.
The case fatality rate of COVID-19 is relatively low (~2%) compared to two other coronaviruses, such as SARS-CoV (15%) and MARS virus (43%) (Hajjar et al., 2013). However, the rapid spreading and high human-to-human transmission have made the disease far more lethal than any other disease in recent history.
More importantly, an increasing body of evidence indicates that a significant number of COVID-19 survivors have been facing multiple health complexities, leaving a massive burden on the health care system in the coming years.
Researchers from Washington University School of Medicine in St. Louis addressed the issue. They found that COVID-19 survivors—including the individuals who did not require hospitalization—have an increased risk of mortality in the six months following diagnosis with the virus.
The study results are published in the journal Nature on July 23, 2021 (Al-Aly et al., 2021).
“Our study demonstrates that up to six months after diagnosis, the risk of death following even a mild case of COVID-19 is not trivial and increases with disease severity,” said senior author Ziyad Al-Aly, MD, an assistant professor of medicine.
“It is not an exaggeration to say that long COVID-19—the long-term health consequences of COVID-19—is America’s next big health crisis.”
“Given that more than 30 million Americans have been infected with this virus, and given that the burden of long COVID-19 is substantial, the lingering effects of this disease will reverberate for many years and even decades.”
“Physicians must be vigilant in evaluating people who have had COVID-19. These patients will need integrated, multidisciplinary care.”
The study calculated the risk of death and severe illness in COVID-19 survivors and compared the findings with control non-COVID patients.
They collected all information about the participants from the national database of 87,089 COVID-19 survivors and 5,004,832 people with influenza. Among the participants, 13,654 people with COVID-19 and 13,997 with influenza were hospitalized and survived for 30 days after hospitalization.
Then, the researchers investigated a wide range of events involving diagnoses, medication, and laboratory tests. They also looked into survivors’ experience following their 30 days post-diagnosis or hospitalization until the end of the six-month follow-up observation period.
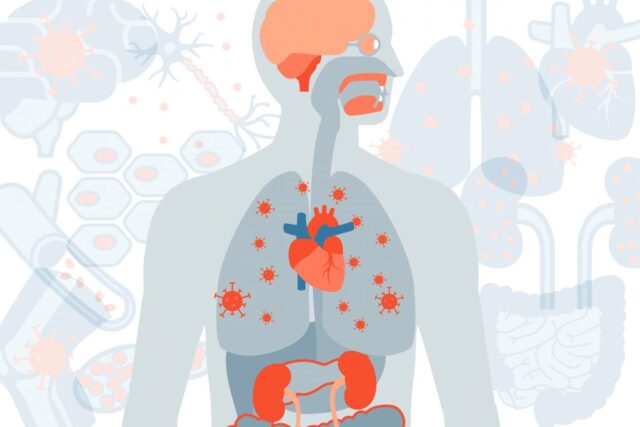
The study looked into a vast database related to multiple organ systems like lung, heart, kidney, stomach, brain, muscle monitoring respiratory problems, chest pain, heart failure, coronary disease, kidney injury, constipation, diarrhea, type-2-diabetes, depression, hyperlipidemia, joint pain, memory problems, obesity, smell disorder, and hair loss.
Giving a broad view on several issues rather than just the neurologic or cardiovascular complications made this study different from other studies, according to the author Al-Aly, also director of the Clinical Epidemiology Center.
The investigators showed that COVID-19 survivors had an almost 60% increased mortality risk during the post-COVID-19 six months compared with the general population.
At the six-month, excess mortality of all COVID-19 survivors was estimated, and the value was eight people per 1,000 patients. Among the hospitalized patients who survived after the first 30 days of illness, the number of excess deaths was 29 per 1,000 patients over the following six months.
The researchers confirmed that though COVID-19 is primarily a respiratory virus, once recovered, a COVID-19 patient may face multiple complexities involving almost every organ system in the body.
After evaluating nearly 379 diagnoses of diseases probability related to COVID-19, 380 classes of medications prescribed, and 62 laboratory examination reports, the researchers identified newly diagnosed significant health issues that COVID-19 patients experienced over at least six months, and that affected nearly every organ and regulatory system in the body (Figure 1)

Compared with flu survivors, COVID-19 survivors had an almost 50% increased risk of death, with about 29 excess deaths per 1,000 patients in six months. COVID-19 survivors also had a substantially higher risk of long-term medical problems.
They also noted that the health risks from surviving COVID-19 increased with disease severity, with patients hospitalized requiring intensive care being at the highest risk of long COVID-19 complications and death.
“Compared with flu, COVID-19 showed remarkably higher burden of disease, both in the magnitude of risk and the breadth of organ system involvement,” Al-Aly said.
“Long COVID-19 is more than a typical post-viral syndrome. The size of the risk of disease and death and the extent of organ system involvement is far larger than what we see with other respiratory viruses, such as influenza.”