Summary
Since the first identification of COVID-19 in China, there has been a rapid increase in cases and death. The pathogenesis remains mostly unknown, and no effective treatment is available yet. The aim of this meta-analysis was to re-look into the case severity associated with hypertension. Methods: A systematic search was conducted in Pubmed, ScienceDirect, and Google Scholar for relevant articles. Retrieved articles were pooled in Endnote X6, and Open-Meta and Review Manager were used for analysis. Results: Thirty-five articles involving 8850 patients have been included in this analysis. Among the patients, the prevalence of hypertension was 24.2% (95% CI: 21.2-27.2%, p < 0.001). The analysis revealed that prevalence of hypertension was significantly higher in severe/mortal patients with risk ratios (RR) 2.19 (95% CI 1.92 to 2.49). Conclusion: Hypertension is a prevalent risk factors in COVID-19 patients, the outcome may help clinicians determine early and appropriate medical management.
Key words: SARS-CoV-2, COVID-19, 2019-nCoV, risks, comorbidity, characteristics
Introduction
Covid-19 is a respiratory disease. Caused by the virus SARS-CoV-2, the disease has imposed immense suffering on the health of the global community. Rapid transmissibility, lack of effective treatment, and lesser-known pathogenicity have made this outbreak the deadliest in recent history.
Despite resemblance with the two other coronavirus outbreak, SARS-2003, and MERS-2012, SARS-CoV-2 virus has significant genetic dissimilarity with two other viruses. Targeting the same respiratory tract, with many common symptoms such as fever, fatigue, dry cough, anorexia, myalgia, dyspnea, SARS-CoV-2 shares genetic identity with SARS-CoV and MERS-CoV 79% and 50%, respectively [1].
Given the increasing number of active cases and insufficient treatment solutions, alternative methods need to be addressed to control the spread of the disease. It is particularly essential to develop the tools to identify risk factors associated with disease severity and poor outcome among infected individuals. Identifying the people at high risk of developing the severity of the disease could help health care professionals improve the quality of the service and effective utilization of the available resource.
This meta-analysis has searched relevant articles and analyzed the prevalence of hypertension related to the poor prognosis of infected individuals.
MethodsA systematic search for data was conducted on Pubmed, ScienceDirect, and Google Scholar from January 1, 2019, to May 5, 2020. The search keywords included 2019‐nCoV, 2019 novel coronavirus, COVID‐19, coronavirus disease 2019, SARS-CoV-2 vs. risk, characteristics, and comorbidity. Studies that presented epidemiology, clinical features, and the prevalence of hypertension in SARS-CoV-2 infected patients were assessed for inclusion in this meta-analysis. In the analysis, the severe group includes the patients who are either diseased, admitted into the ICU, or otherwise described severe in the records. Non-severe group included who were alive and did not fall in the criteria mentioned above.
All data analyses were performed on OpenMeta Analyst (version windows 7) and RevMan version 5.3. Pooled results of proportion at their respective 95% confidence intervals (CI) presented in the analysis were calculated using the DerSimonian–Laird method. The pooled results of risk ratio (RR) were calculated at their respective 95% CI using the Mantel–Haenszel method. Heterogeneity was assessed by Cochran’s Q test.
Results
The search retrieved 121 articles, of which 25 were duplicates. After reviewing the title and abstract, 56 records were considered for full-text review. Finally, 35 articles were found consistent for full inclusion criteria. A total of 8850 people from the 35 selected studies were enrolled in this meta-analysis. All studies were conducted in China.
[table id=1 /]
This meta-analysis for the identified studies compared the prevalence of hypertension among severe and non-severe patients. In the comparison analysis, a random effect model was applied because of higher heterogeneity (I2>50%).
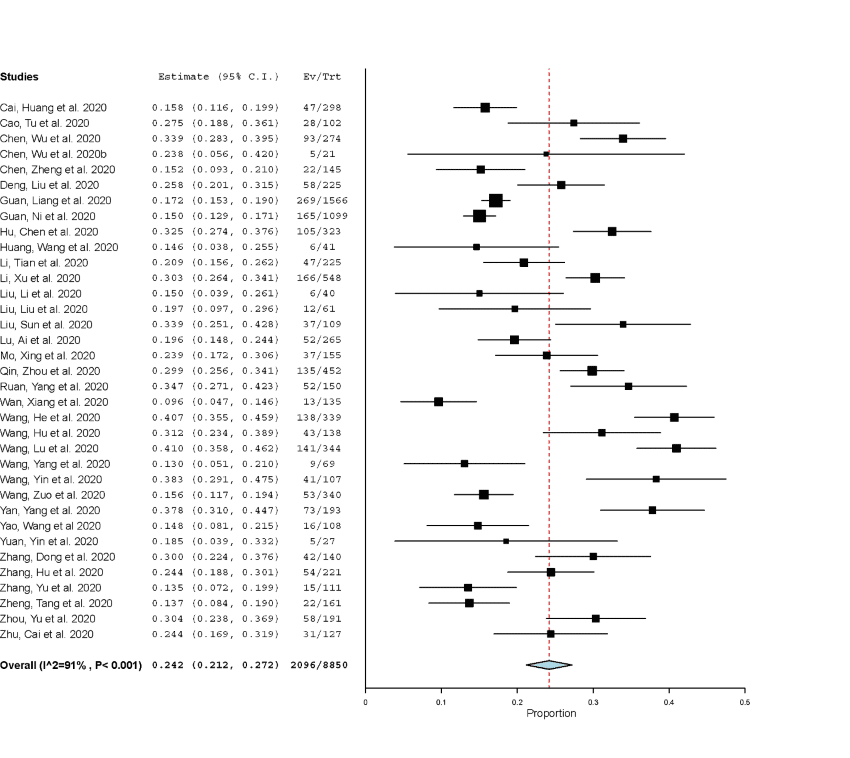
O f the total 8850 cases, 2527 patients were found in severe group. Data, as analyzed on the OpenMeta platform, revealed that prevalence of hypertension was 24.2%, (95% CI: 21.2-27.2%, p<0.001), Figure 1. The analysis also found that patients with previous hypertensive conditions accounted for 39.4 % of the severe patients, the value was, on the other hand, 17.6% among non-severe patients. The proportion in severe cases compared with the non-severe cases was statistically significant (RR 2.19, 95% CI 1.92 to 2.49; I2 = 58%), as shown in Figure 2.

Discussion
Coronaviruses are enveloped viruses, have a single-strand positive-sense RNA of 26 to 32 kb in length within its structures. The family, called Coronaviridae, has at least seven strains of coronavirus. Two of them caused severe respiratory illness in humans in the past. First, SARS-CoV, during the 2002-2003, infected 8,096, and killed 774 people in 29 territories/countries [37]. Second, MARS-CoV, which evolved in the Middle East infected 2519 people, killed 866 in 27 countries with case fatality 34.3% [38]. In the middle of December, in 2019, the virus that caused acute respiratory outbreak in Uhan, China, has killed over 350,000 people as of May 25, 2020. A high number of scientific reports, have been published on this topic, as well. It is crucial to message the main findings of the clinical characteristics of COVID-19 through a comprehensive review of the existing evidence, notably by narrow down the topic, focusing on the most vulnerable people of the society who are at the greatest of risk of this pandemic.
In this review, critical clinical findings reported in 35 original articles that assessed the prevalence of hypertension on severe and non-severe COVID-19 cases were extracted, synthesized, and then analyzed. The analysis found that the overall prevalence of hypertension in the infected people was 24.2% (95% CI, p< 0.001), which is in accordance with the prevalence of hypertension (23.2%) among the Chinese population [39]. Therefore, this analysis did not find people with hypertension were more susceptible to SARS-CoV-2 infection. However, when the prevalence of hypertension is assessed among severe and non-severe COVID-19 patients, the analysis found more severely infected people had a higher proportion of hypertension (39.1%), which is 2.2-fold higher than in the non-severely infected people.
The underlying mechanism behind the propensity is evolving at a high pace. It sometimes contradicts one analysis to another, even though there is a broad consensus that people with comorbidity like hypertension and cardiac diseases are at high risk of falling on the horizon of death row.
The involvement of ACE2 receptor specificity has been speculated to be the primary reason for the severity of this disease. SARS-CoV-2 virus, like SARS-CoV-1, binds with the same ACE2 receptor to get entry into the cells [40]. This receptor is widely expressed in lung, cerebrovascular tissue, kidney, and stomach. This receptor is also shown to be overexpressed in the response of ACEI/ARB’s drugs often used to treat hypertension and other forms of the cardia-cerebrovascular disease. Therefore, increased expression of ACE2 could, at least theoretically, increase binding the virus to the lung and other tissues, and aggravate its pathophysiological effect in the patients. One included study has shown that mortality rates of patients with and without the use of ACEI/ARBs were 36.8% (7 of 19) and 25.6% (43 of 168) [41]. Though the ACE2 dependent severity is often argued, as the enzyme ACE2, reduces the inflammatory action of angiotensin II by converting it to inactive angiotensin 1-7. Therefore, the use of ACEI/ARBs could be beneficial to treat COVID-19. Nonetheless, some studies have shown that the use of ACEI/ARB did not influence morbidity or mortality [42]. As casualties in the treatment group were 7.7%, 42 of 545 patients, compared with the patients 23 of 279 (8.2%) who did not receive the drugs [43], ACEI/ARB is suggested to use in SARS-CoV-2 infections [44].
Another model explaining the relationship between hypertension and COVID-19 severity has involved cholesterol—a marker of coronary heart disease. As reported in 2008, a closely related virus SARS-CoV-1 requires cholesterol and monosialotetrahexosylganglioside1 (GM1) lipid domains (GM-1 lipid rafts) for infectivity in cultured cells. It is also possible that other factors facilitate the entry of SARS-CoV-2 in the lung or other affected cells. In a laboratory test, one study found that cells loaded with cholesterol-rich lipoprotein A (apoE) enhance the endocytic entry of pseudotyped SARS-CoV-2 [45] .
Conclusion
A total of 8850 COVID-19 cases were included in this meta-analysis. Of these, 2527 cases were considered severe. Individuals with hypertension had 2.2 to 2.4-fold higher risk compared with their non-severe counterparts. Further, this meta-analysis supports the notion that the pathogenicity of SARS-CoV-2 infection may not be limited to ACE2 receptor susceptibility. High levels of tissue cholesterol play a significant role in the development of the disease.
This meta-analysis is not beyond any limitations. Apart from the sample size, assessment of severity, quality of data, and patients with another comorbidity in the assessment influence the conclusion. Nonetheless, the information provided will further enrich knowledge about this critical disease and improve patients’ outcomes and lower the fatality rate.
The author declares no conflict of interest.
Author: Molay Roy, PhD; Orchid ID: 0000-0002-8236-7265
© 2020 sciencetrend.ca | All rights reserved |



















